Osteoporosis CME Insights: A Review of New Clinical Practice Guidelines

Osteoporosis-related bone loss can progress silently for years or even decades. In contrast, osteoporosis treatment guidelines are updated frequently, offering new strategies for reducing fracture risk and improving patient outcomes.
Dr. Kashif Piracha, a double board-certified physician in internal medicine and nephrology, explores the latest osteoporosis guideline updates from the American College of Physicians (ACP). Piracha serves as an academic hospitalist at Houston Methodist Willowbrook Hospital in Texas, internal medicine clerkship director for Texas A&M College of Medicine, and fellow of the American College of Physicians, American Society of Nephrology, and National Kidney Foundation.
New ACP guidelines highlight a stronger push to treat osteoporosis more proactively, citing the millions at risk and the new research and availability of proven, cost-effective treatments. “It’s a silent disease, and there is renewed urgency because osteoporosis is taking a toll on the population as a whole,” says Dr. Piracha. With quality continuing medical education, you can stay current and help close treatment gaps that contribute to that toll.
Why Osteoporosis Deserves Your Attention
To understand the urgency in treating osteoporosis more effectively, we need only to look at the data. The cost of caring for osteoporotic fractures is estimated to reach $95 billion by 2040. Osteoporosis accounts for more hospitalizations than myocardial infarction, stroke, or breast cancer.
“On top of that, only about 20% of patients who have an osteoporotic fracture receive proper secondary prevention to prevent another fracture. If you compare that with patients with cardiac disease or heart attack, almost 95% of those patients get secondary prevention,” says Dr. Piracha. “And we have to take into account the mortality that is caused by osteoporosis. Roughly 30% of patients with osteoporosis die within one year of having a fracture, and that’s devastating. A lot of it can be preventable if we employ the right treatment strategies.”
Stay Current With the Latest Guidelines
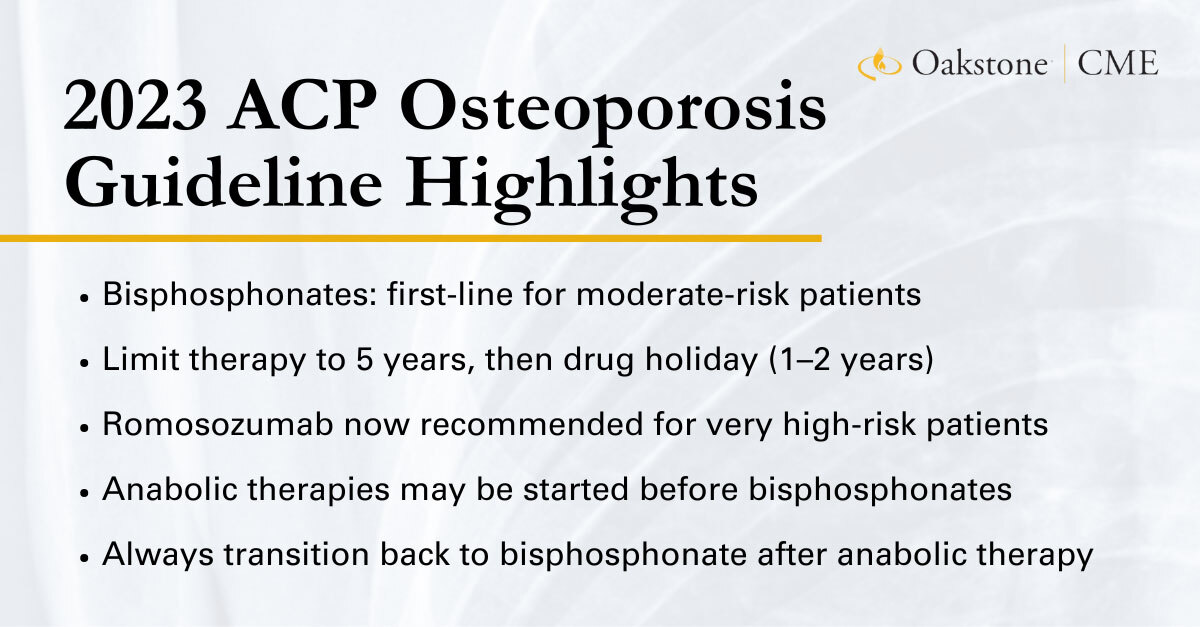
With these facts in mind, the ACP released updated osteoporosis guidelines in 2023. Dr. Piracha highlights three of the most notable differences.
“Bisphosphonates were recommended back in 2017, but now we have more data that these medications are absolutely vital,” he says. The ACP now strongly recommends the use of bisphosphonate as the primary drug to treat postmenopausal women with osteoporosis and men with osteoporosis, so long as the risk of fracture is moderate.
However, bisphosphonate use should be limited to five years. The ACP’s evidence-based advice indicates a bisphosphonate drug holiday for most patients at moderate risk of osteoporotic fractures. “Bisphosphonates are amazing drugs for osteoporosis, but obviously, like any other drug, they have side effects,” says Dr. Piracha.
Anabolic therapy recommendations are also a significant new addition. “We have evidence that anabolic therapies are more potent and can give better results in patients with very high osteoporotic disease,” Dr. Piracha adds. “The important point to note is that romosozumab, which is part of the recommendation now, is a new addition. The drug wasn’t even around in 2017, when the last guidelines were made.”
Refining Osteoporosis Care: New Guidance on Drug Selection and Timing
The most recent osteoporosis management guidelines have refined the order of recommended therapies for specific populations while also establishing a treatment timeline.
“We now have recommendations that we can use anabolic therapies first before using bisphosphonates, and we can use these anabolic therapies in very high-risk patients,” says Dr. Piracha. “And then after they have been treated with anabolic therapies, we can switch them to bisphosphonates.”
Overall, these new drugs give physicians more options for effective treatment, Dr. Piracha adds.
Prime candidates for first-time bisphosphonate therapies will be those at moderate risk of fracture. These typically include patients with diagnosed osteoporosis, fragility fracture at the hip or spine, osteopenia, or on chronic steroid therapy.
The transition from one treatment to the other “is actually pretty simple,” Dr. Piracha says. “If a patient is on bisphosphonate therapy, you can just stop the bisphosphonate on one day and then, the next day, start an anabolic agent like teriparatide.”
He adds that patients taking denosumab may experience bone mineral loss, as the earliest stages of teriparatide treatment increase bone turnover.
The Drug Holiday Debate: Timing and Monitoring
The evidence for transitioning patients between bisphosphonates and anabolic therapies goes beyond personal preference.
“It has been shown that treating with bisphosphonates for longer than five years does not give any significant additional benefit for nonvertebral fractures,” says Dr. Piracha. “It actually increases the risk of atypical femoral fractures and increases the risk of osteonecrosis of the jaw.”
That’s why ACP recommends pausing bisphosphonate treatment after five years. For optimal long-term management of osteoporosis, this drug holiday lasts one to two years, and patients should have a low to moderate risk of fracture before switching therapies. Anabolic therapies are the most common and effective osteoporosis treatment during this holiday, with a caveat.
“You cannot use anabolic agents forever. The duration of therapy with teriparatide is recommended to be two years. For romosozumab, the treatment duration is one year,” says Dr. Piracha. “Once you’ve completed treatment, you’ve got to put the patients back on bisphosphonate therapy. Otherwise, whatever bone mineral density gains you have achieved are going to be lost.”
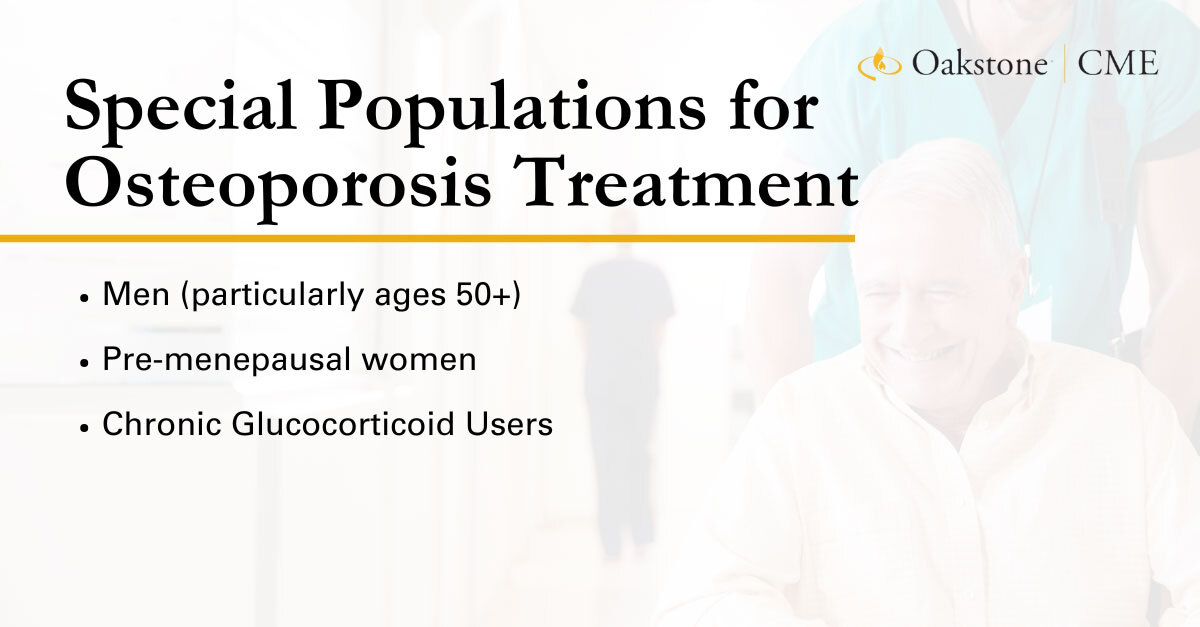
Don’t Overlook Special Populations
As with most medical conditions, osteoporosis affects underserved or often overlooked populations. “Osteoporosis has traditionally been regarded as a disease of women,” notes Dr. Piracha, “so therefore a lot of patients — a lot of doctors, even — don’t pay as much attention to their male patients for osteoporosis.”
Osteoporosis in men is fairly common. Up to one in four men over 50 will develop an osteoporotic fracture in their lifetime, and men are twice as likely as women to die in the two years after a hip fracture. The Endocrine Society has long recommended that any man over the age of 70 should have a dual-energy X-ray absorptiometry test for bone mass.
Other at-risk populations include patients taking prednisone long term and premenopausal women, too. Osteoporosis isn’t as common among these patient populations, but the risk shouldn’t be overlooked. Maintaining CME credits can help combat pervasive medical myths and ensure that patients receive the right osteoporosis treatment at the right time.
Stay Ready for What’s Next in Osteoporosis
Dr. Piracha emphasizes the importance of screening at-risk populations. “Don’t miss the diagnosis of osteoporosis,” he says. “What’s most important for primary care physicians is to make sure that they stay updated on the latest happenings in the field of osteoporosis. There are going to continue to be more changes in the future, so we want to make sure there are no practice gaps.”
There’s a lot to learn, but osteoporosis CME designed for on-the-go physicians can keep you current on the latest advancements. Oakstone’s flexible recorded evidence-based content, practical reviews, videos, audio, and mobile-friendly training are available anytime. Stay ahead and close practice gaps with the latest CME osteoporosis updates.